Notch Therapy: A New Approach to Tinnitus Treatment
Leanne Powers, AuD, Gisele Munhoes dos Santos, PhD, Catherine Jons, AuD
AudiologyOnline, October 13 2016
Introduction
Tinnitus affects a staggering number of individuals. Population studies conducted in six different countries reported the incidence of prolonged tinnitus varying between 4.4 and 15.1 percent for adults. One study reported 2.4 percent of the population responded “yes” to the description of tinnitus as “tinnitus plagues me all day” (Moller, 2011).
Tinnitus not only causes a decreased quality of life for some individuals, but is also a health issue with an economic impact (Wunderlich et al., 2015). In the U.S., tinnitus is the most common service-related injury (Department of Defense Centers for Hearing Excellence Statistical Data, 2016) affecting more than 800,000 US veterans (U.S. Department of Affairs, 2016). With such a prevalent epidemiology, it is not surprising that many hearing instrument manufacturers have added tinnitus treatment options.
Acoustic treatment for tinnitus produced by ear-worn instruments began in 1976 when sound-therapy devices were first introduced. The treatment was based on the principle of distraction, turning total masking with white noise into a clinical management technique (Vernon, 1976). In the 1990s, the concept of “habituation” was introduced. Jastreboff and Hazell (1993) defined a neurophysiologic model of tinnitus, which led to the development of Tinnitus Retraining Therapy (TRT; Jastreboff & Jastreboff, 2000). TRT commonly uses ear-level worn noise generators and hearing instruments, or a combination of the two devices (i.e., dual function of amplification, as well as therapy noise generator) to help facilitate the natural process of habituating to the tinnitus. The TRT protocol is only one of several tinnitus treatment regimens recommending sound-therapy devices (Powers & Munhoes, 2015).
Hearing instruments (with or without a sound generator component) are a mainstay of the audiologic management of tinnitus (Hoare, Searchfield, Refaie, & Henry, 2014). Hearing aids are considered the number-one treatment to help the tinnitus patient manage their tinnitus, even when their hearing loss is mild (Baguley, 2016). Surr and colleagues (1985) surveyed 200 new hearing instrument wearers and found 62 percent of the respondents reported tinnitus. Of these individuals, approximately half noted either a partial or total relief from tinnitus secondary to wearing the hearing aids. The respondents further reported the relief from tinnitus was an important contributor to wearer satisfaction.
More recently, the American Academy of Otolaryngology created guidelines that included the use of hearing instruments as tinnitus treatment (Tunkel et al., 2014). These guidelines are supported by current survey data. MarkeTrak VIII revealed nearly two out of three respondents reported hearing aids relieved their tinnitus most of the time to all of the time, while three out of ten reported that hearing aids alleviated their tinnitus all of the time (Kochkin, Tyler, & Born, 2011). A retrospective study by Searchfield and colleagues (2010) concluded that amplification plus counseling provided twice the reduction in tinnitus handicap over counseling alone. Habituation through acoustic therapy (which usually includes wearing hearing instruments) can be applied to all types of tinnitus, and therefore is the treatment method of choice for many hearing care professionals.
For individuals who present with tonal tinnitus, that is, the perception of a near-continuous sound or overlapping sounds with a well-defined frequency (American Tinnitus Association), an alternative to habituation therapy is available. Tonal tinnitus is present in the majority of individuals with tinnitus. A joint comprehensive tinnitus study conducted by the Kresge Hearing Research Laboratory and the University of Oregon Health Sciences Center Tinnitus Clinic revealed that tinnitus pitch falls largely into two broad categories: tonal and noise. Their research found that more than half of the subjects, or 59 percent, reported tonal tinnitus, 25 percent reported noise-type tinnitus, and 16 percent presented with a combination. The subjects were further classified based on frequency of the tinnitus. A near two-thirds, or 63 percent, indicated perceiving tinnitus between 2000 and 7000 Hz. Only 21 percent had low-tone tinnitus below 2000 Hz, and 16 percent had tinnitus above 7000 Hz (Turner, 1990).
New research supports attempts to mitigate tonal tinnitus from its anatomic origin utilizing spectral notching rather than treating the effects of tinnitus through traditional habituation noise therapy. This paper will discuss a novel approach of utilizing hearing instruments employing notch-modified acoustic output to treat patients with tonal tinnitus.
Anatomy and Physiology of Tinnitus – Review
From an anatomical perspective, three underlying mechanisms that cause tinnitus have been proposed: 1.) changes in the level of spontaneous neural activity in the central auditory system; 2.) changes in the temporal pattern of neural activity; and, 3.) reorganization of tonotopic maps (Lanting, de Kleine, & van Dijk, 2009).
Tinnitus is now widely accepted as a brain disorder as opposed to the traditional paradigm viewing it as an ear disease. A hearing loss in the auditory periphery is likely necessary, but not essential, for tinnitus to occur. Animal studies have shown that cochlear damage due to traumatizing sounds, ototoxic drugs, or other means produces significant changes in the central auditory pathway. One change is a reorganized tonotopic map, with cortical neurons in the hearing loss region being tuned to the edge of the normal hearing region. Another change is an overall hyperactivity in the central auditory pathway from cochlear nuclei to auditory cortices, including increased spontaneous activity, increased serial synchrony or bursting firing within a nerve fiber, and increased spatial synchrony between nerve fibers. Because decreased spontaneous and driven activity is typically observed at the auditory nerve level in response to cochlear damage, this central hyperactivity ― a hypothesized neural correlate of tinnitus ― may reflect increased central gain (Reavis, Chang, & Zeng, 2010).
Current working models describing the origin of tinnitus support a top-down versus bottom-up elevation of neural activity or a combination of both top-down involving the central nervous system and bottom-up, the peripheral auditory system (Melcher, 2016). The loss of peripheral sensory input or cochlear function is thought to be responsible for a spontaneous increase in neural activity from the damaged area of the cochlea, spontaneous activity coming from the peripheral auditory system, or bottom-up. However, subsequent gain increase, secondary to this spontaneous activity, causes synchronized activation of neural fibers and can be perceived as “tonal tinnitus” (Wunderlich et al., 2015). The increase in gain is most likely a top-down processes. Contributing to the synchronized activity is a lack of lateral inhibition in the auditory cortices (Wunderlich et al., 2015). Lateral inhibition is “a process in which the most active sensory nerve fibers in a bundle… inhibit action potentials in adjacent fibers from the periphery of the stimulus area” (definition per http://medical-dictionary.thefreedictionary.com/).
Acoustic trauma has been linked with changes in synaptic inhibition in the damaged areas of the cochlea. The auditory deprivation creates an excitation-inhibition imbalance throughout the central auditory pathway, most likely from a weakening of the inhibitory network surrounding this area (Teismann, Okamoto, & Pantev, 2011). It has been proposed that providing additional stimulation to the affected area (hearing loss frequencies) effectively “evens out” the imbalance and reduces the perception of tinnitus (Eggermont, 2012). Even with the advanced hearing instruments available today, providing adequate stimulation to achieve this goal is not always possible. As an alternative, efforts to reduce the loudness perception of tonal tinnitus turned to the use of music therapy. Okamoto introduced a notched-music method during which subjects listened to self-chosen, enjoyable music notched to remove energy in the frequency range surrounding the tinnitus frequency (Okamoto, Stracke, Stoll, & Pantev, 2010).
Utilizing Spectral Notching to Treat Tinnitus
The theory behind notched music therapy contends that music, modified with a spectral notch, reduces cortical activity corresponding to the center frequency (CF) of the notch. The CF is identified by conducting a clinical pitch-matching procedure. The procedure typically involves presenting audible tones of varying frequencies using a bracketing A-B-A comparative approach in which the patient chooses the pitch that most closely represents “their tinnitus tone” (Okamoto et al., 2010). Since notched therapies typically use a bandwidth filter between 0.5 and one full octave, an exact match to the perceived tinnitus pitch is not necessary (Wunderlich et al., 2015). Customized notching of music is thought to increase lateral inhibition while providing a pleasant stimulus that helps ease the limbic system reaction to tinnitus (Pantev, Wolbrink, Roberts, Engelien, & Lutkenhoneret, 1999). These findings serve as the foundation for tailor-made notched music training (TMNMT) (Strauss, Corona-Strauss, Haab, & Hannemann, 2015).
Results of a 12-month TMNMT study revealed a significant reduction in both subjective tinnitus loudness and tinnitus-related auditory cortex evoked potentials, as measured by magnetoenchalography (MEG) and auditory steady state response (ASSR), when compared to both a control and placebo groups (Okamoto et al., 2010). Okamoto and colleagues (2010) concluded changes in the tonotopic organization of the auditory cortex are based on neurons being excitable by frequencies other than their original source region. This results from damage (hearing loss) in the source region. The reorganization is characterized by a lack of inhibitory networks which may lead to synchronized neural firing over the auditory cortex perceived as tinnitus. Notching creates spectral edges to the deprived frequency band of the cochlea, which helps to suppress the neural hyperactivity by increasing lateral inhibition (Strauss et al., 2015). A spectral edge frequency (SEF) is a measurement of signal processing; the SEF is the frequency below which 75-95 percent of the total power of the signal is located. It is posited that the lower edge of the notch contributes most to the increased inhibition of the perceived tinnitus pitch.
One limitation to TMNMT is that the individual is required to allocate time on a daily basis to listen to the notched therapy music. This involves dedication to the program and disrupts normal daily routine. Further, TMNMT fails to address the amplification needs of the patient.
Signia Notch Therapy
Hearing aids like Signia primax™ offer a variety of tinnitus treatment options to meet the individual needs of any patient. It is up to the clinician to decide the best course of treatment for each individual based on the patient’s type of tinnitus and various additional factors. Signia hearing instruments offer a traditional habituation approach with various static therapy signals to choose from: White Noise, Pink Noise, Speech Noise, High Tone Noise, and Brownian Noise. These static therapy choices can be further individualized by custom shaping with respect to frequency content if desired. Additionally, four modulated Ocean Wave signals are available for patients who prefer a more dynamic sound. With the launch of Connexx 8.2 fitting software, tinnitus treatment options available in primax instruments have been expanded to include Notch Therapy.
Signia Notch Therapy (NT) is a new therapy approach. Based on the concept of “re-attracting” lateral inhibition (Teismann, Okamoto, & Pantev, 2011), Notch Therapy uses spectral notching and applies it to the principles of traditional amplification with hearing instruments. Amplification has been clinically proven to reduce patient scores on the Tinnitus Handicap Inventory and subjectively reduce the impact of tinnitus in daily life (Sweetow & Sabes, 2010, dos Santos et al., 2014). Therefore, NT aims to attack tinnitus on two fronts: 1.) enhancing the auditory environment by amplification to compensate for hearing loss, and 2.) suppressing the tinnitus-associated neural hyperactivity with enhanced lateral inhibition.
Strauss and colleagues (2015) conducted a double-blind study to determine the subjective and objective efficacy of using notched environmental sound technology (NEST) with individuals reporting tonal tinnitus (NEST being the original name for Signia Notch Therapy). Subjects included 20 individuals with mild hearing loss and distressing tinnitus, as defined by the Tinnitus Questionnaire 12 (TQ12), an assessment questionnaire that identifies tinnitus-related psychological distress.
TQ12 is comprised of twelve questions, 0-24 points, to assess tinnitus distress. A score of 0-5 (degree 1) equates to slight distress, 6-10 (degree 2) indicates medium distress, 11-15 (degree 3) signifies severe distress, and 16-24 (degree 4) is classified as very severe distress. The TQ12 has a re-test reliability value of 0.89 (Hiller & Goebel, 2004). Mean age for the study was 53 years. In addition to standard audiometric testing, the tinnitus frequency was identified using a frequency matching technique in conjunction with a visual analog scale. Subjects were randomly assigned to one of two groups. Group 1 was fit with commercially available behind-the-ear hearing instruments and Group 2 was fit with the same instruments, but with the notched environmental sound technology activated. The TQ12 was administered at the beginning of the study and repeated at three weeks to assess the subjective effects of NEST.
EEG and auditory late responses (ALR) measures were used to objectively assess the therapy. Neural long-term habituation (l-hab) has been shown to correlate to the ALR and used as a way to quantify tinnitus distress (Strauss et al., 2015). It is believed that tinnitus sufferers have an l-hab deficit, which makes it difficult to habituate to the acoustic stimulus used during the ALR testing, particularly in the area of the tinnitus frequency. The loss of automatic attention to the ALR stimulus (e.g. 1 kHz tone), is demonstrated by a reduction of the wavelet phase stability (WPS) in the ALR response. The decrease in WPS is correlated to a decline in selective auditory attention. To quantify the therapeutic effect of Notch Therapy, the l-hab gain factor is computed as the difference between pre- and post-therapy. The larger the difference, the more long-term habituation improves.
Results indicated a more predominant improvement for the NT approach, as defined by an improvement in the TQ12 score. This improvement was clearly shown after only three weeks, with percent of benefit corresponding to Cohen’s d value of 0.84 (Strauss et al., 2015). Similarly, the mean l-hab gain factor increased for Group 2, suggesting improved habitation to the stimulus tone used during the ALR measurements. This efficacy study shows that this approach positively impacts the tinnitus sufferer by increasing habituation and decreasing distress levels within a three-week post-therapy window. Figures 1 and 2 depict the outcomes of the pilot study (Strauss et al., 2015) in which Group 1 was the control group with traditional amplification and Group 2 had amplification with the therapy notch enabled. The mean improvement of four points in the notch group reflects an improvement of the tinnitus distress level by one complete category.
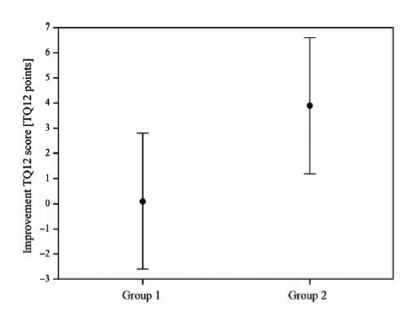
Figure 1. Tinnitus Questionnaire 12 (TQ12) represents the change in points from pre-study evaluation score to the post-study outcome score. Group 1 (control) showed virtually no improvement with an average point improvement score of zero, while Group 2 (NT) showed an average improvement of four points.
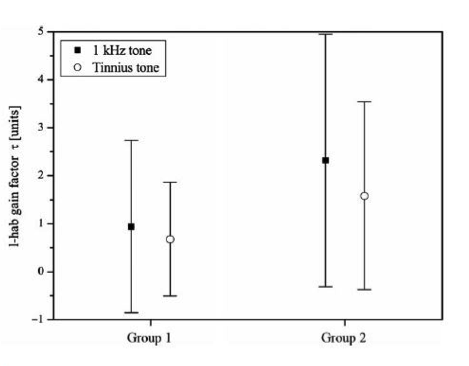
Figure 2. Mean l-hab gain factor improvement (-1 to 5) for a 1 kHz signal and tinnitus tone relative to the pre-therapy evaluation. Note that the objective results show improvement for both groups as l-hab factors increased. However, a larger improvement is seen in Group 2.
A follow-up, double-blind study was conducted to determine the subjective and objective long-term effectiveness of Signia NT. Subjects included 34 individuals with mild-to-moderate hearing loss and well-documented subjective, chronic tinnitus. Mean age was 56.5 years. Subjects were divided into two groups. Group 1 was fit with commercially available, digital-processing behind-the-ear hearing instruments and Group 2 with the same hearing instruments, but the output signal was spectrally notched at the individual tinnitus frequency identified using a standard frequency-matching procedure. Notch width was 0.5 octave centered at the perceived tinnitus pitch. All subjects completed the Tinnitus Questionnaire 52 (TQ52) at the beginning of the study, after three months, and after six months of therapy. Like the TQ12, the TQ52 assesses tinnitus severity, but in a more comprehensive manner. Minimal clinically important difference (MCID) in the TQ52 score is about -5 points for an improvement and +1 point for deterioration (Adamchic et al., 2012). EEG and ALR measures were used to objectively assess the therapy.
Results of the subjective assessment indicated a prominent improvement in the TQ52 scores at the three-month point for the notched environmental sounds approach. An improvement in the TQ52 score translates to a reduction of tinnitus-related distress. Improvement of the target group, relative to the control group, show that the significant decrease in TQ52 score for Group 2 is maintained at the six-month evaluation (Figure 3). Statistical analysis revealed the notch group to exhibit a medium-to-large improvement compared to the conventionally fit group. This is indicated to be an effect size (Cohen’s d) of 0.49 after three months and 0.62 after six months.
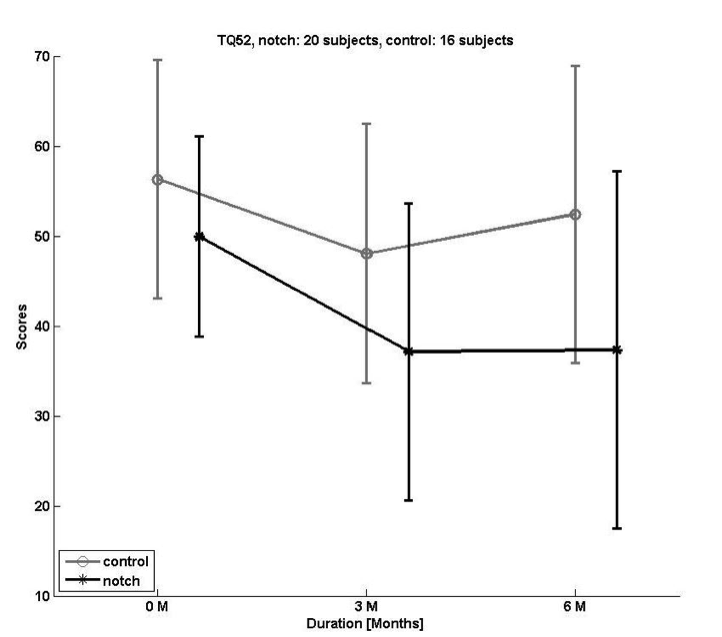
Figure 3. Average reduction of Tinnitus Questionnaire 52 (TQ52) scores for Group 1 (Conventional Fitting) and Group 2 (Notched Fitting). A reduction of the TQ52 score corresponds to an improvement in tinnitus perception and relief. Group 1, the control group, demonstrated a maximum improvement at three months, lessening at six months. Group 2 demonstrated a significant reduction in TQ52 scores at three months and this improvement sustained through the six-month study period.
Percent benefit based on (TQ52) scores at three and six months are shown in Figure 4. Group 1 (Conventional Fitting) achieved roughly 15 percent benefit at three months, but declined to 7 percent benefit at six months. Group 2 (Notched Fitting) achieved a 26 percent benefit (approximately 10 percent more than the Conventional Fitting) at three months, and importantly, maintained that improvement through the six-month evaluation. At six months, the Notched Fitting group demonstrated a TQ52 benefit of more than 17 percent greater than the Conventional Fitting group.
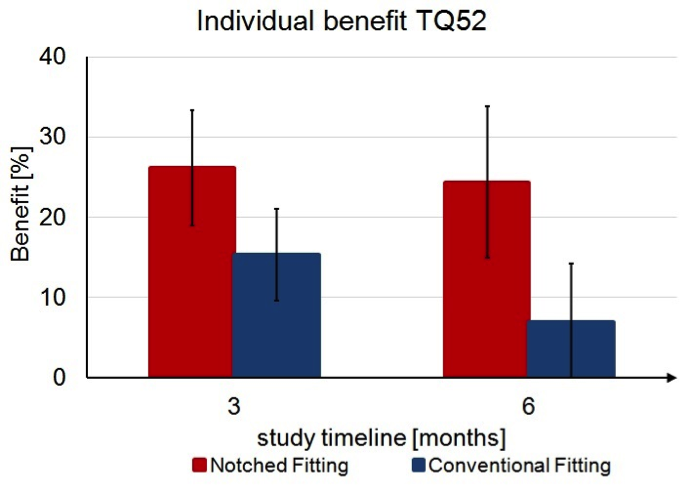
Figure 4. The percent benefit based on Tinnitus Questionnaire 52 (TQ52) scores at three and six months. Represented in blue Group 1 (Conventional Fitting) and shown in red Group 2 (Notched Fitting). Group 2 achieved roughly 10 percent more benefit at three months, which was maintained through the six month completion of the study.
Additionally, the TQ52 benefit seen was independent of perceived tinnitus frequency. In Figure 5, the TQ52 benefit is shown in percentage as a function of perceived tinnitus frequencies for each individual in the Notched Fitting group. Pearson and Spearman correlation test confirmed no significant correlation between the reported pitch of the subjects percent of benefit from NT.
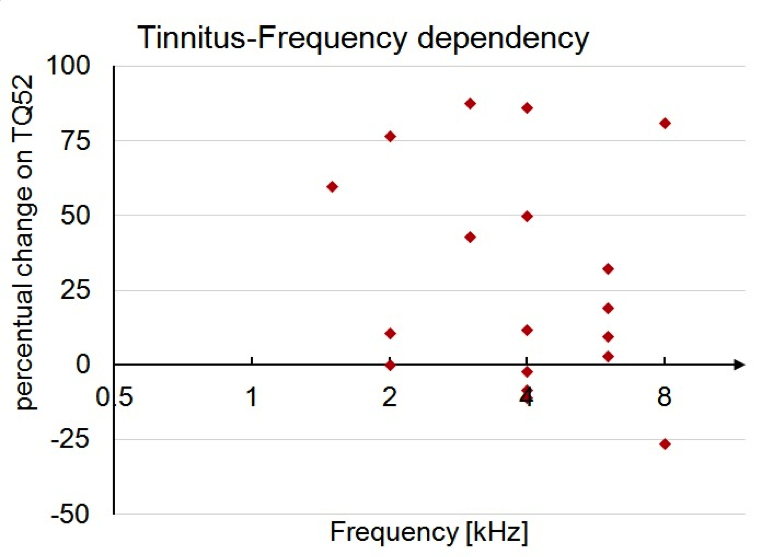
Figure 5. Percent of benefit at six months in relationship to the individual tinnitus frequency in the Notched Fitting group.
NT results were also independent of hearing loss. TQ52 is shown in Figure 6 as percent benefit in relation to the degree of hearing loss. The lack of data-point clustering indicates the degree of hearing loss was not a factor in predicting the outcome for NT. This was confirmed by the Pearson correlation test that showed no significant correlation between degree of hearing loss and benefit from NT.
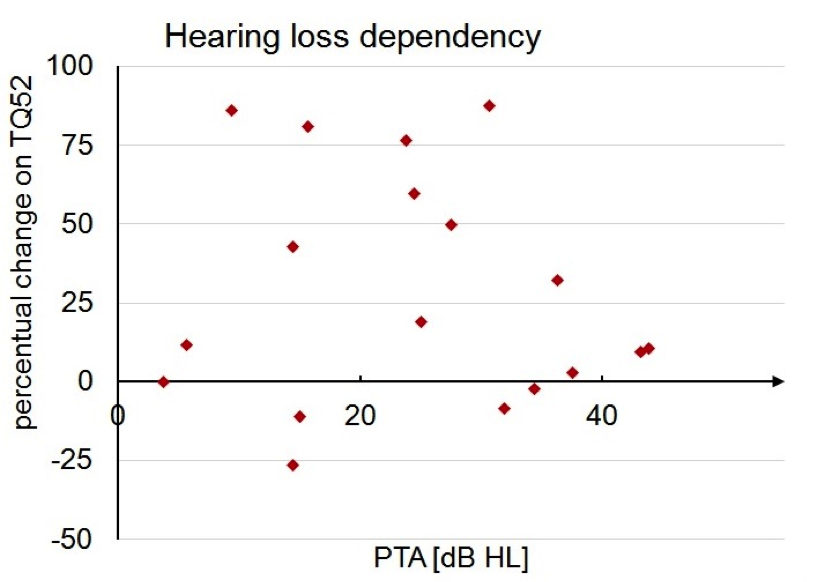
Figure 6. The x-axis is the pure tone average (PTA) for the Notched Fitting group and the y-axis shows percent of benefit seen on the Tinnitus Questionnaire 52 (TQ52) confirming no relationship between degree of hearing loss and the percent of benefit from Notch Therapy at six months.
Results of the objective measures indicated an increase in l-hab gain for the Notched Fitting group when compared to the control group at three months with an even greater difference evident after six months, indicating an improved ability to habituate to the tinnitus (Figure 7).
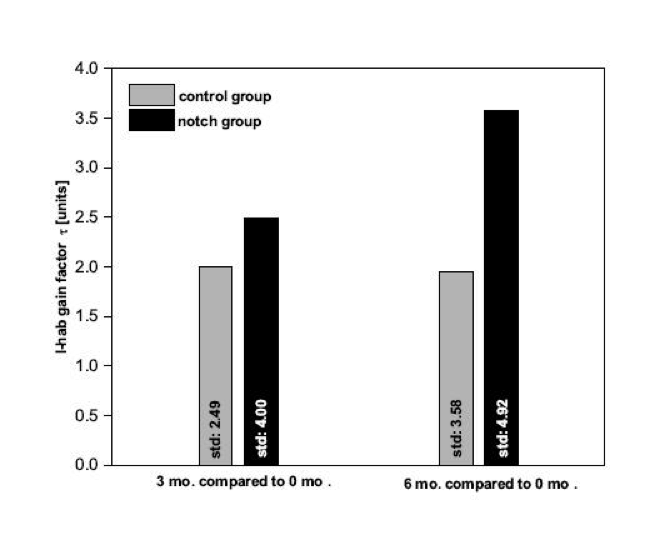
Figure 7. Mean objective habituation marker development for three and six month’s post-therapy. The bars indicate the average habituation factor as measured with EEG. The data for the y-axis is expressed as long-term habituation gain, with 0.0 representing no habituation ability and 4.0 indicating the ability to habituate to the presented tone. Group 1 (control with traditional amplification) is represented by the gray bars and Group 2 (Notch Therapy) is represented by the black bars. Standard deviations are given in text format inside the respective bar. Note that standard deviations originate in large part from ALR morphology shifts due to stimulus adaptation and can be reduced by grouping the patients according to their tinnitus frequency (Haab et al., in submission)
The study provided the following conclusions:
- There appears to be a therapeutic advantage of implementing Notch Therapy compared to amplification alone.
- There is no additional “therapy” time needed with NT compared to TMNMT (Okamoto et al., 2010).
- NT was shown to be effective for patients with mild-moderate hearing loss and tonal tinnitus even when the tinnitus was characterized as severe, chronic, pure-tone tinnitus (Hannemann, Haab, Corona-Strauss, & Strauss, 2016).
Implementation of Notch Therapy
Signia primax hearing instruments offer NT as software based tinnitus therapy option in the Connexx® 8.2 fitting module (for details of the implementation and recommended workflow, refer to Wolf, 2016). The NT option is in addition to the traditional tinnitus therapy already offered to assist with the habituation approach to tinnitus management.
In order to activate NT, the clinician needs to determine the placement of the notch by a simple pitch-matching procedure. Connexx offers three options for determining and entering the pitch that most closely represents the patient’s perceived tinnitus tone. The generally recommended method is to use the Guided Matching procedure. The clinician plays two tones (A & B) to the patient through their primax hearing instruments. The patient indicates which tone is closer to their perceived tinnitus pitch. This process is repeated several times as Connexx automatically narrows the frequency range to identify the most appropriate pitch match. A sample screen shot is shown in Figure 8.
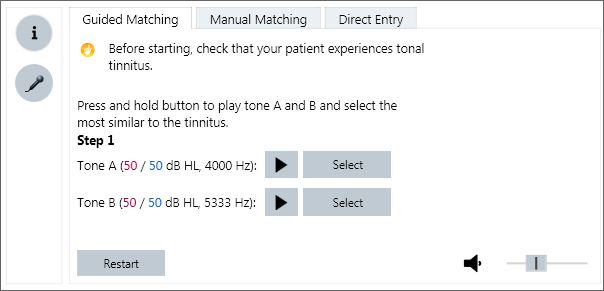
Figure 8. Screen view of the three tinnitus pitch-matching procedures available in the Connexx 8.2 fitting software. Shown is the Guided Matching selection.
The second approach available is Manual Matching (see Figure 9). Using this procedure, the clinician presents tones through the primax hearing aids to obtain a pitch match through a more traditional pitch matching procedure (Henry, Zaugg, & Schechter, 2005). The clinician manually adjusts the frequency and intensity of the presented tone through the software similar to the operation of an audiometer.

Figure 9. Screen view of the three tinnitus pitch matching procedures in Connexx 8.2 fitting software. Shown is the Manual Matching selection.
The third method, Direct Entry, allows the clinician to enter an already determined tinnitus frequency as the pitch match. Some clinicians may have performed a tinnitus pitch match either with their audiometer or with some other form of equipment designed for this assessment. For those clinicians, Connexx Direct Entry option allows the choice of 31 different frequencies. The clinician should choose the frequency closest to the tinnitus frequency they have already identified and select “use frequency” as seen in Figure 10.
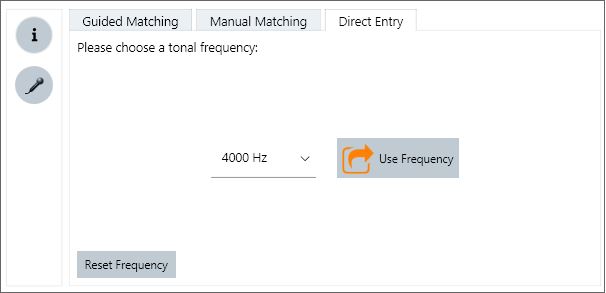
Figure 10. Screen view of the three tinnitus pitch matching procedures in Connexx 8.2 fitting software. Shown is the Direct Entry selection.
To confirm the appropriate pitch match was found, a Frequency Check needs to be completed prior to initiation of the notch, regardless of which pitch matching option was used. The Frequency Check is shown in Figure 11.
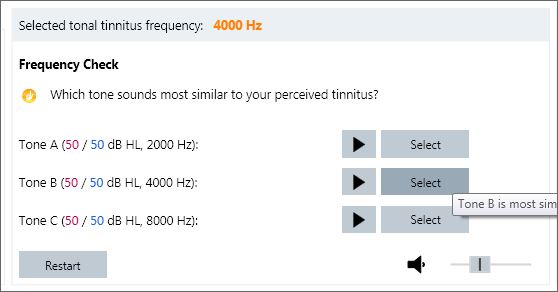
Figure 11. Screen view in Connexx 8.2 software showing the Frequency Check.
Once the frequency is confirmed with the Frequency Check, the clinician selects in which programs to activate the notch. Placing the notch in all programs is recommended. The width of the notch is only 0.5 octaves and therefore should not interfere with speech understanding. However, the option of choosing to active specific programs “notch free” is provided for flexibility and individualized therapy. In the event a patient desires a program using only traditional amplification, the clinician should leave that program unchecked. The data suggests that longer wearing times are better than shorter, particularly in those cases when the prescribed gain is minimal, and therefore the resulting notch depth is shallower. A complete screenshot of the Tonal Tinnitus view is shown in Figure 12.
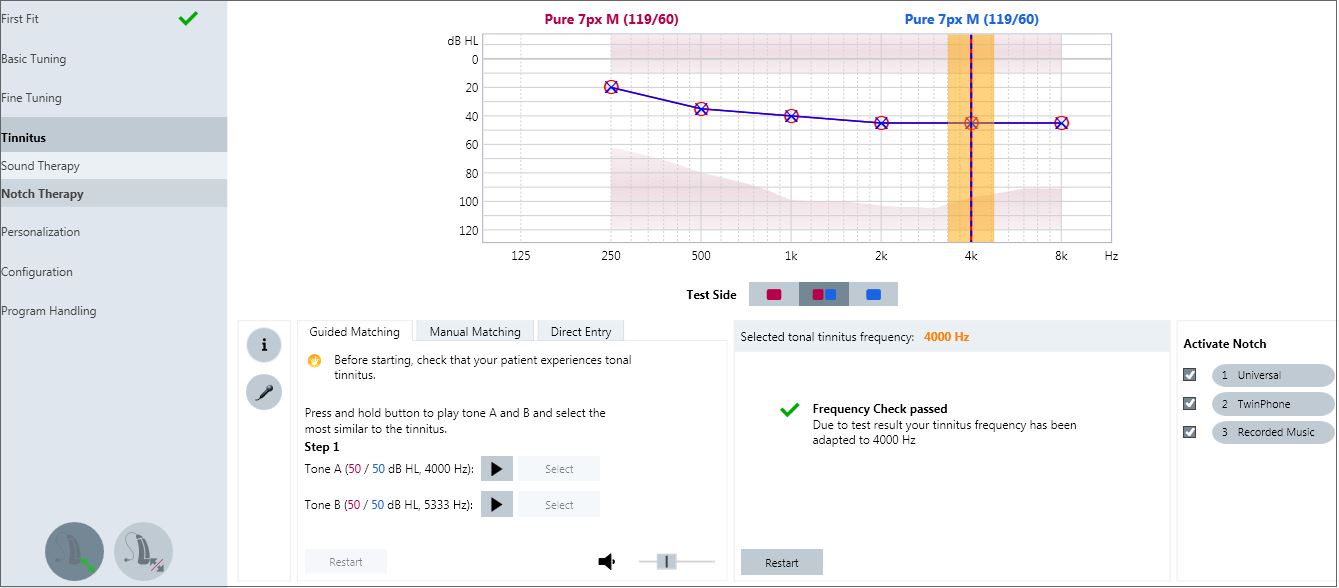
Figure 12. Tonal Tinnitus Therapy screen in Connexx 8.2 showing a manually entered pitch match as 3333 Hz, with the Frequency Check completed and the notch activated in all three listening programs.
Conclusion
Notch Therapy is a new tool developed by Signia, which has been clinically proven as an effective treatment for tonal tinnitus. With Notch Therapy, the notched frequency response provides a therapeutic effect by spectrally modifying the acoustic signal while integrating seamlessly into the wearer’s personal amplification. NT is implemented continuously throughout the wearer’s daily routine, negating the need to set aside time for the tinnitus therapy. Tinnitus perception is decreased by enhancing the acoustic landscape through amplification while simultaneously encouraging lateral inhibition through the use of a spectral notch. By adding a Notch Therapy option, Signia offers the most comprehensive and flexible combination device available for tinnitus treatment.
References
Adamchic, I., Tass, P.A., Langguth, B., Hauptmann, C., Koller, M., Schecklmann,…Landgrebe, M., (2012). Linking the tinnitus questionnaire and the subjective clinical global impression: Which differences are clinically important? Health and Quality of Life Outcomes, 10, 79.
American Tinnitus Association (n.d.). Retrieved Sept 9, 2016 from https://www.ata.org/understanding-facts/symptoms
Baguley, D., (2016). Clinical aspects of tinnitus. Hearing Review, 23(1), 40.
dos Santos, G.M., Bento, R.F., de Medeiros, I.R., Oiticcia, J., da Silva, E.C., & Penteado, S. (2014). The influence of sound generator associated with conventional amplification for tinnitus control: randomized blind clinical trial. Trends in Hearing, 18, 1-9.
Eggermont, J. (2012) Cortex: Way station or locus of the tinnitus percept? In J. Eggermont, F. Zeng, Popper, R. Fay (Eds.), Tinnitus (137-162). New York, NY: Springer Science+Business Media.
Haab, L., Lehser, C., Corona-Strauss, F., Bernarding, C., Seidler, H., Strauss, D., & Hannemann, R. (in submission). Six-month evaluation of a hearing aid supported tinnitus treatment using notched environmental sounds.
Hannemann, R., Haab L., Corona-Strauss, F., & Strauss, D. (2016, September). Long-term evaluation of a new hearing aid supported tinnitus treatment. Poster presented at the meeting of the World Congress of Audiology, Vancouver, Canada.
Henry, J.A., Zaugg, T.L., & Schechter, M.A. (2005) Clinical guide for audiological tinnitus management I: Assessment. American Journal of Audiology, 14, 21-48.
Hiller, W. & Goebel, G. (2004). Rapid assessment of tinnitus-related psychological distress using the Mini-TQ. American Journal of Audiology, 43(10), 600-604.
Hoare, D.J., Searchfield, G.D., Refaie, A.E., & Henry, J. (2014). Sound therapy for tinnitus management: J Am Acad Audiol. 2014 Jan;25(1):62-75. doi: 10.3766/jaaa.25.1.5.
Jastreboff, P. & Hazell, J. (1993). A neurophysiological approach to tinnitus: Clinical implications. British Journal of Audiology, 27, 7-17.
Jastreboff, P. & Jastreboff, M. (2000). Tinnitus retraining therapy (TRT) as a method for treatment of tinnitus and hyperacusis patients. J Am Acad Audiol, 11(3), 162-177.
Kochkin S., Tyler R., & Born, J. (2011). MarkeTrak VIII: The prevalence of tinnitus in the United States and the self-reported efficacy of various treatments. Hearing Review, 18(12), 10-27.
Lanting, C.P., de Kleine, E., & van Dijk, P. (2009, September). Neural activity underlying tinnitus generation: Results from PET and fMRI. Hearing Research, 225(1-2), 1-13.
Melcher, J. (2016). Tinnitus: A multifaceted condition. Audiology Today, 28(1), 32-37.
Moller, A.R. (2011). Epidemiology of tinnitus in adults. In A.R. Moller, B. Langguth, D. DeRidder, & T. Kleinjung (Eds.), Textbook of tinnitus (29-37). New York, NY: SpringerScience+Business Media, LLC.
Okamoto, H., Stracke, H., Stoll, W., & Pantev, C. (2010). Listening to tail-made notched music reduces tinnitus loudness and tinnitus-related auditory cortex activity. Proceedings of the National Academy of Sciences, 107(3), 1207-1210.
Pantev, C., Wolbrink, A., Roberts, L.E., Engelien, A., & Lutkenhoner, B.B. (1999). Short-term plasticity of the human auditory cortex. Brain Research, 842(1), 192-199.
Powers, L., & Munhoes, G. (2015). Acoustic therapy for the treatment of tinnitus: A primer. Hearing Review, 22(6), 22.
Reavis, K,. Chang J., & Zeng, F. (2010). Patterned sound therapy for the treatment of tinnitus. The Hearing Journal, 63(11), 21-24.
Searchfield, G.D., Kaur, M., & Martin, W.H. (2010). Hearing aids as an adjunct to counseling: Tinnitus patients who choose amplification do better than those that don’t. International Journal of Audiology, 49(8), 574-579.
Strauss, D.J., Corona-Strauss, F.I., Haab, L., & Hannemann, R. (2015). Notched environmental sounds: a new hearing aid-supported tinnitus treatment evaluated in 20 patients. Clinical Otolaryngology, [Epub ahead of print]. doi: 10.1111/coa.12575
Surr, R.K., Montgomery, A.A, & Mueller, H.G. (1985). Effect of amplification on tinnitus among new hearing aid users. Ear Hear, 6(2), 71-5.
Sweetow, R.W., & Sabes, J.H. (2010). Effects of acoustical stimuli delivered through hearing aids on tinnitus. J Am Acad Audiol, 21(7), 461-473.
Teismann, H., Okamoto, H., & Pantev, C. (2011). Short and intense tailor-made notched music training against tinnitus: The tinnitus frequency matters. PLoS ONE, 6(9). e24685. doi:10.1371/journal.pone.0024685
Tunkel, D.E., Bauer, C.A., Sun, G.H., Rosenfeld, R.M., Chadrasekhar, SS., Cunningham, E.R….Whamond, E.J. (2014). Clinical practice guideline: tinnitus. Otolaryngology–Head and Neck Surgery, 151(2S), S1–S40. doi: 10.1177/0194599814545325
Turner, J.S. (1990). Auditory dysfunction: tinnitus. In H.K. Walker, W.D. Hall, & J.W. Hurst (Eds.), Clinical methods: The history, physical, and laboratory examinations. Boston: Butterworths.
United States Department of Affairs (n.d.). Retrieved Sept 13, 2016 from http://www.research.va.gov/topics/hearing.cfm
Vernon, J. (1976). The use of masking for relief of tinnitus. In H. Silverstein & H. Norrell (Eds.), Neurological Surgery of the Ear: Volume II (104-108). Birmingham: Aesculapius Publishing.
Wolf, V. (2016). How to use primax tinnitus therapy options. Signia Whitepaper.
Wunderlich, R., Lau, P., Stein, A., Engell, A., Wollbrink, A., Rudack, C., & Pantey, C. (2015, September). Impact of spectral notch width on neurophysiological plasticity and clinical effectiveness of the tailor-made notched music training. PLoS ONE, 10(9).


