Supporting hearing health and general health with My WellBeing
Niels Søgaard Jensen, Brian Taylor
Introduction
The World Health Organization (WHO) defines health as “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity” (WHO, 1948). The definition has received some criticism since its creation, mainly because the use of the word “complete”, which means that the definition “would leave most of us unhealthy most of the time” (Smith, 2008). Despite the criticism, however, the WHO definition makes some thoughtful points, including that health is a multidimensional entity that involves components of physical, mental, and social health. Further, given the relationship between these important components of health to hearing, it is critical hearing care professionals take a holistic view of patient well-being.
For decades, hearing health has – roughly speaking – been defined mainly by the pure-tone audiogram, which divides people into groups with either normal hearing or various degrees of hearing loss. For persons with hearing loss, the provision of hearing aids is the primary way to compensate for this condition. For generations, Signia technology has benefitted millions of hearing aid wearers in their everyday life. With the continuous development and launch of new and groundbreaking audiological features and form factors, Signia continues to be a leader in the quest for innovative solutions.
Today, however, it is simply not enough to look at hearing health and hearing loss in isolation. To view hearing aids as the sole tool for hearing-loss treatment – and as a means of only compensating for hearing loss – in shortsighted. Mounting research has shown that hearing loss is more than an isolated condition. Instead, it is associated with many other physical, mental, and social facets of a person’s general health. These advances in how we understand the links between hearing loss and general health have affected the development of new technology in a big way, and Signia hearing aids now offer many features beyond those of ‘just’ amplifying sounds to compensate for hearing loss.
With the launch of My WellBeing, which tracks key parameters related to both hearing loss and general health, Signia has taken another major step towards addressing the hearing aid wearer holistically, and not simply as an ear with hearing loss. This paper is divided into two parts. Part one describes the background of My Wellbeing, the links between hearing loss and other health dimensions, and how hearing aids play a crucial role – not only for hearing-loss compensation but also for the general health and well-being of the wearer. Part two of the paper introduces My WellBeing, outlines some of its benefits, and discusses how it contributes to both the hearing aid wearer’s hearing health and general health.
PART 1: Linking hearing loss and general health
Connections between other health conditions and hearing loss
Hearing loss has a number of comorbidities (e.g., Abrams, 2017; Besser et al., 2018), i.e. other chronic diseases that coexist with hearing loss. Some comorbidities exist in isolation because, like hearing loss, they become more prevalent with age (e.g., back pain). Thus, these types of comorbidities are usually not affected by hearing loss. In contrast, other comorbidities are more directly linked. However, the causal relationships are not always clear, often because there are other complicating factors making the links difficult to study. Below are some examples of comorbidities linked to hearing loss.
Among the health conditions linked to hearing loss are cardiovascular disease (e.g., Tan et al., 2018) and diabetes (e.g., Samocha-Bonet et al., 2021). While there may be some uncertainty regarding the causal relationships of these conditions to hearing loss, there are plausible explanations why they negatively affect hearing. We know, for example, that cardiovascular disease reduces the blood flow to the inner ear, and the abnormal blood sugar levels associated with diabetes damage the small blood vessels and nerves in the inner ear. In both cases, damage to the auditory system may result and cause hearing loss.
Hearing loss is also linked to cancer, either directly, where the presence of an ear tumor can cause the hearing loss, or indirectly, where the treatment of cancer damages cochlear hair cells. An example of the latter is the chemotherapy drug, cisplatin, which is intended to kill cancer cells, but is often ototoxic (Schacht et al., 2012).
Negative effects of hearing loss on health and well-being
Hearing care professionals (HCPs) have a vested interest in knowing how hearing aids might affect the complex relationship between hearing loss and other dimensions of health. To better understand both the primary and secondary effects that hearing loss has on other health conditions, considerable research has been conducted.
Figure 1 shows a simplified model of how age-related hearing loss (presbyacusis) affects other health-status components (functional capacities, physical state, psychological well-being, and social relations), which all contribute to a person’s overall health-related quality of life (QoL; WHO, 1997). The figure illustrates that age-related hearing loss may result in withdrawal, reduced cognition, and declining physical and social activity. Additionally, since the factors work in combination, a vicious circle may be created in which QoL further erodes.
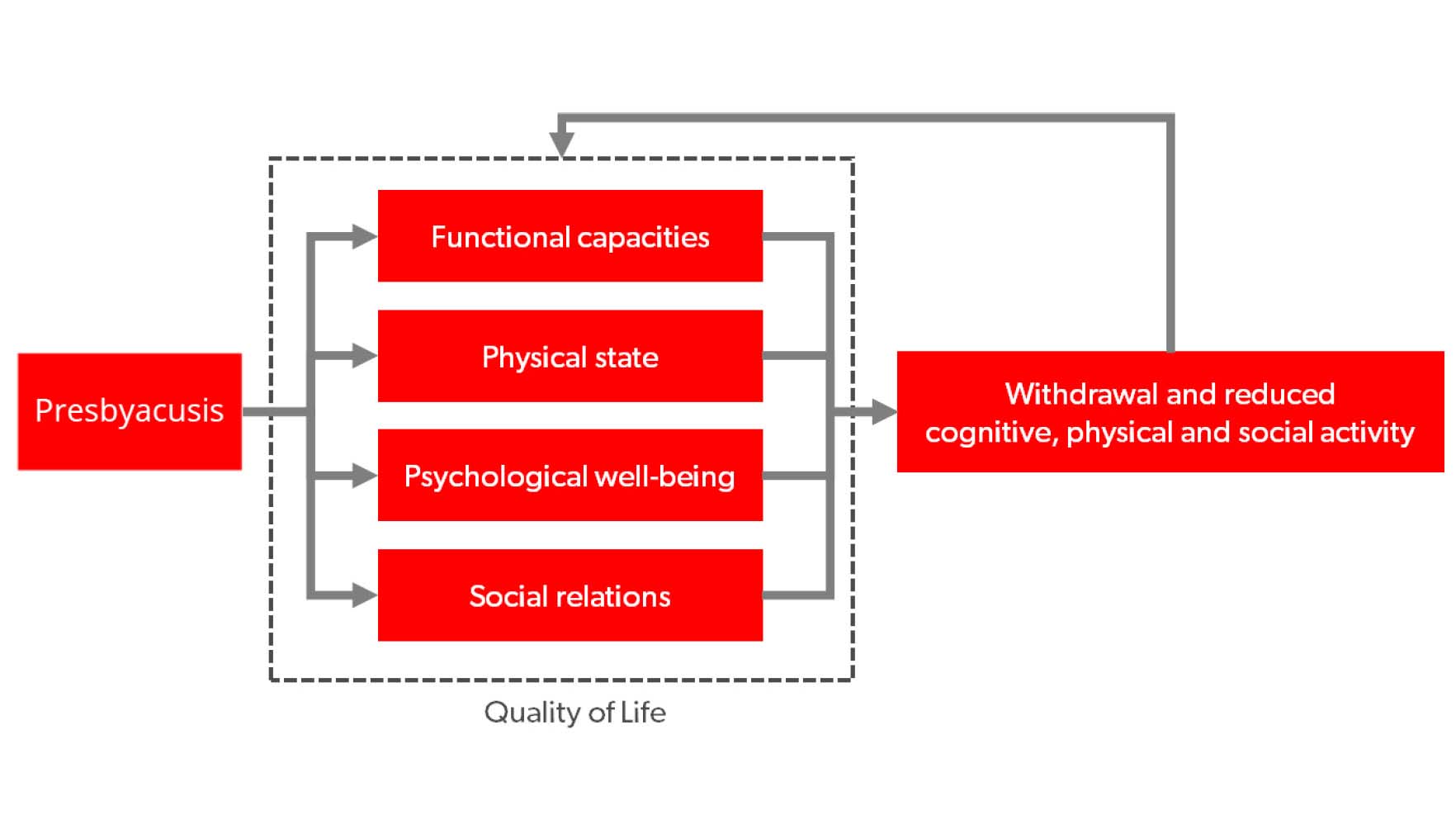
Figure 1. Simplified model of how age-related hearing loss (presbyacusis) can affect different components contributing to the overall health-related quality of life (QoL). This can result in withdrawal and reduced cognitive, physical, and social activity, which may further negatively impact the QoL components. The figure is partly based on WHO (1997).
The first component affected by hearing loss in Figure 1 is functional capacities, which refers to the capability of performing tasks and activities that people find necessary or desirable in their lives. When sounds are inaudible it becomes difficult or even impossible to understand speech in certain situations, everyday activities, tasks, and jobs become difficult to perform, and functional capacity is reduced. For example, Tye-Murray et al. (2009) reported that some professionals in the workforce expressed “a sense of having lost their competitive edge” directly as a consequence of their hearing loss, e.g., when having problems talking on the phone. In another domain of functional capabilities, hearing loss can be associated with an increased risk of falling. One possible explanation of this association between hearing loss and falling is that hearing loss limits access to auditory cues needed for environmental awareness (Lin & Ferrucci, 2012).
The next component affected by hearing loss in Figure 1 is physical state, which covers a multitude of health dimensions. For example, hearing loss can lead to increased listening fatigue in everyday life, which results in reduced QoL (Holman et al., 2021b; Davis et al., 2021) Studies also have suggested hearing loss is associated with poorer physical function with aging (Martinez-Amezcua et al., 2021) and a poorer physical activity profile (Kuo et al., 2021).
One topic that has received considerable attention in recent years is the impact of hearing loss on cognition, see Powell et al. (2022) for a recent overview. Several studies and reviews have linked hearing loss to accelerated cognitive decline and dementia (e.g., Lin et al., 2011; Amieva et al., 2015; Thomson et al., 2017). Thus, even though the underlying mechanisms are still not fully understood, it is by now well-established that untreated hearing loss increases the risk of cognitive decline. Further, hearing loss is now considered the largest potentially modifiable risk factor for age-related dementia (Livingston et al., 2020; WHO, 2021). Among the possible explanations of why hearing loss can have a detrimental effect on cognition is that prolonged auditory deprivation (i.e. the brain being deprived of sound) affects areas of the brain used for higher-level cognitive processing (Powell et al., 2022).
The final two components in Figure 1, psychological well-being and social relations, are closely related to each other. Both components are related to the psychosocial consequences of hearing loss. The communication difficulties caused by an untreated hearing loss and the consequences of functioning in social and professional contexts can, for example, cause social isolation, depression, anxiety and negatively impact family relationships. See Shield (2019) for an overview of the social consequences of hearing loss. It is also well-established that hearing loss has a number of socioeconomic consequences, both for the individual and for society (WHO, 2017; Shield, 2019).
While this section only scratches the surface of the relationship between hearing loss and other conditions, it should be clear that hearing loss is strongly connected to several dimensions of health and wellness. The obvious question every HCP should ask is: What happens when we treat hearing loss? We know properly fitted hearing aids will improve communication abilities, but how do hearing aids affect the other health conditions linked to hearing loss? And how do hearing aids affect the general health and well-being of a person? Those questions are addressed in the following section.
Positive effects of wearing hearing aids
The core purpose of hearing aids is to compensate for hearing loss, and the immediate direct effect for the wearer is improved communication abilities. Equally important, however, are the cascading benefits of prolonged and consistent hearing aid use.
Both research and clinical experience suggest hearing aid use results in several other health-related benefits for the wearer. Several studies report health-related benefits associated with hearing aid use along many of the domains outlined in Figure 1. These published findings include improved overall health-related quality of life (e.g., Ferguson et al., 2017), less perceived social and emotional loneliness (e.g., Weinstein et al., 2016), reduced listening-related effort and higher levels of social activity (e.g., Holman et al., 2021a), as well as reducing the risk of falls in older adults (Rumalla et al., 2015).
The potential benefits of hearing aid use on cognition have been discussed extensively in the literature in recent years. A number of studies have shown the prevalence of cognitive decline and dementia is lower in groups of people who use hearing aids, when compared to age-matched groups with untreated hearing loss (e.g., Maharani et al., 2018; Amieva et al., 2018; Byun et al., 2022). However, there is still debate regarding the causal relationship between hearing aid use and the reduction of cognitive decline (Sanders et al., 2021). This is due, in part, to the lack of randomized controlled trials, which is the optimal way to investigate causality. Unfortunately, for ethical reasons, these types of studies are difficult to conduct because they involve withholding treatment to a control group. Thus, we do not (yet) have the evidence to conclude that hearing aids reduce cognitive decline and prevent or slow down the development of dementia (Powell et al., 2022). However, the results cited above are so strong the Lancet Commission and others encourage the use of hearing aids to reduce the risk factor for dementia (Livingston et al., 2020; Byun et al., 2022).
The benefits associated with hearing aid use are related to the number of hours per day hearing aids are worn. Houmøller et al. (2022) found that the self-reported satisfaction with hearing aids increased with daily wear time for both new and experienced hearing aid wearers. Previous studies, summarized by Wong et al. (2003) indicate a similar trend: overall hearing aid satisfaction tends to be higher in those wearing their hearing aids 6 or more hours per day.
There also seems to be an association between the time spent wearing hearing aids and the daily activity level of the wearer. By analyzing logged data from 44,746 fittings of Signia Augmented Experience (AX) hearings aids, retrieved from the Signia Connexx fitting software, a positive correlation between the logged average daily wear time and the share of the wear time spent being physically active, as detected by the built-in motion sensor (Branda & Wurzbacher, 2021), was found. This relationship is shown in Figure 2 where the average wear time is plotted as function of the share of the wear time where physical activity was detected. Note there is a dramatic increase (of more than two hours) in the average wear time when going from a share of 0% (not being physically active at all) to a share of just 1%. When the share of time being physically active further increases, there is a steady increase in wear time until the curve flattens for activity shares higher than 30%. Across all fittings in the data set, the average daily wear time was 9.0 hours, which is slightly above the European average of 8.4 hours reported by Laureyns et al. (2020).
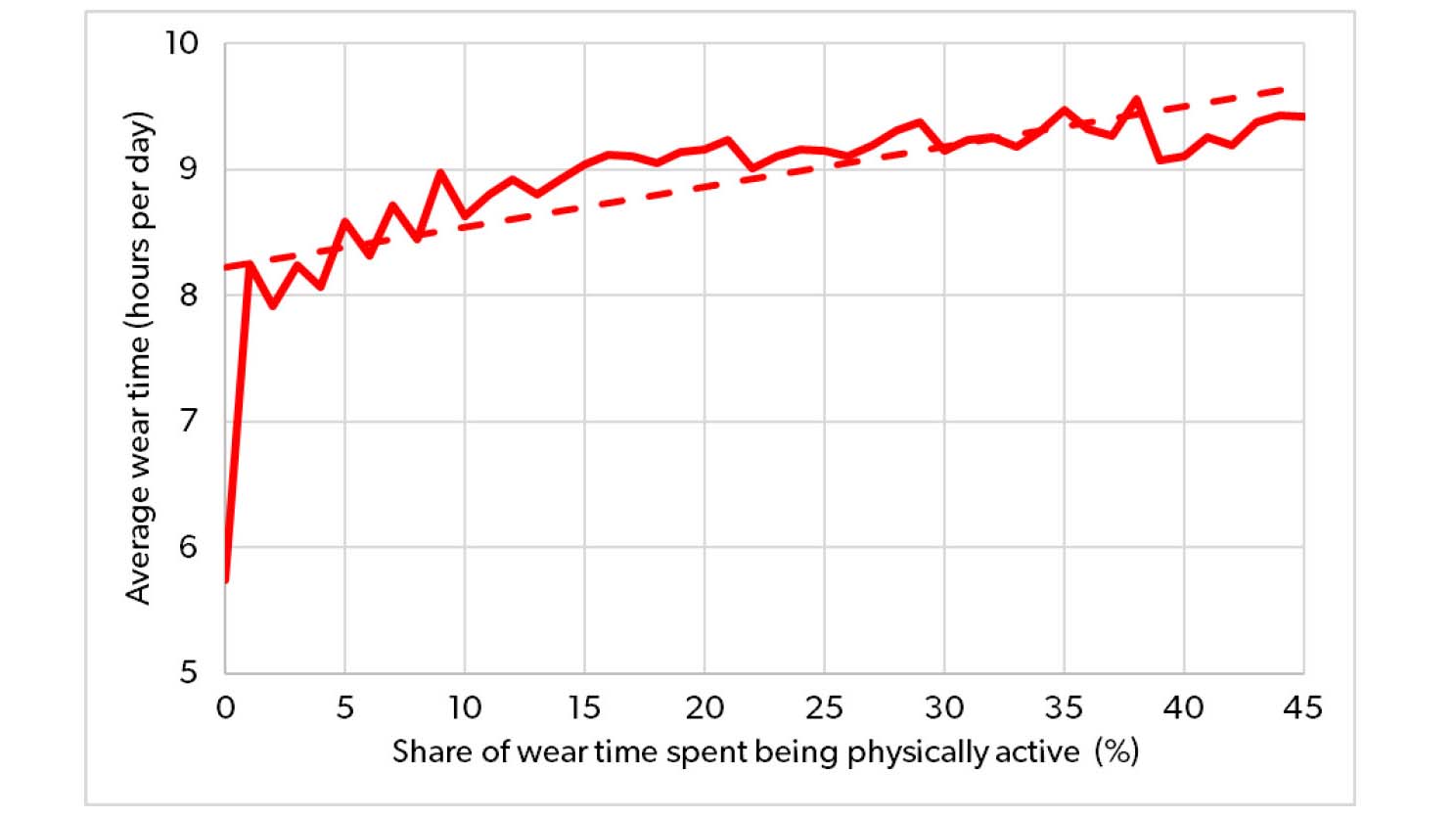
Figure 2. Average wear time plotted as function of the share of the wear time spent being physically active, based on sample of 44,746 Signia AX fittings. A dotted linear regression line has been added to the plot to show the general trend.
Another interesting finding on wear time was made by Williger & Lang (2015) who found that when hearing aids are worn more often, participants reported greater satisfaction and exposure to more diverse listening situations. While the causal relationship in these findings may be unclear, they support an association between hearing aid wear time and daily activity level. This relationship between wear time and daily activity levels indicates that HCPs should encourage all wearers to increase the number of hours per day they use their devices if they want to increase their daily activity levels.
Positive effects of physical activity
The list of positive effects of physical activity – and the risks associated with physical inactivity – is extensive and well-known. There is pool of evidence unambiguously demonstrating that regular physical activity prevents several chronic diseases and other conditions, (e.g., cardiovascular disease, diabetes, cancer, hypertension, obesity, depression, anxiety, stress and osteoporosis) and premature death (e.g., Warburton et al., 2006; Pedersen & Saltin, 2015). Thus, regular physical activity is part of virtually every science-based recommendation on how to achieve or maintain health and well-being.
While it is not considered a primary effect, physical activity has the potential to affect hearing by increasing the blood circulation in the inner ear and thereby strengthening cochlear hair cells. Further, studies show that individuals with good cardiovascular health experience a slower decline in hearing acuity than persons with poor cardiovascular fitness level (Alessio & Marron, 2014). While the group effect is small, and the individual variance is large – with numerous examples of people having perfectly normal hearing without ever exercising as well as extremely active people with a rapidly growing hearing loss – it is still worth noting this direct connection between physical activity and good hearing acuity.
The WHO offers several specific recommendations on the amount of physical activity people ideally engage in on a daily or weekly basis (WHO, 2020). However, it should be noted that WHO also states that doing some physical activity is better than doing none. Arem et al. (2015) showed that the largest relative reduction in mortality risk is obtained when going from not moving at all to moving just a little. Thus, being physically active is more than strenuous workouts and long runs. It can be as simple as brief, casual walks. Just getting up from the couch and moving around in the house or garden also makes a difference to health and well-being.
It is of course interesting that hearing loss and physical activity – besides being directly linked – are related to similar health conditions. This observation emphasizes that hearing health is strongly connected to general health. More than improving communication, it is crucial for HCPs to take the overall health and well-being of help seeking individuals into considerations when fitting hearing aids to consider more than just hearing health when treating hearing loss. This is the rationale behind the introduction of My WellBeing, described in the second part of this paper.
PART 2: My WellBeing
Why My WellBeing?
My WellBeing offers solutions to help Signia AX wearers increase the wear time of their hearing aids and stay healthy. My WellBeing is based on the knowledge and insights presented in Part 1. Data from a range of studies that underscore how hearing loss and treatment of hearing loss are closely connected to general health. Given the abundance of findings in the literature, My WellBeing leverages the importance of physical and social activity to the overall health and well-being of the hearing aid wearer.
As outlined in Part 1, hearing aid use offers several health benefits for people with hearing loss – beyond the basic benefit of improving the ability to communicate: being physically and socially active is a major contributor to a person’s health and well-being. The health tracking features included in My WellBeing act as a valuable tool in encouraging wearers to use their hearing aids more consistently and keep track of health indicators regarding their physical activity. Given that the longer hearing aids are worn during the day, the more accurate the features become, use of My WellBeing may provide extra motivation for using hearing aids more consistently.
How it works
My WellBeing is integrated in and easily reached via the Signia App. When the hearing aids are worn, entering My WellBeing will allow the wearer to immediately get the current daily status on the outcome measures provided by the four features (see Figure 3):
1) My Steps – the number of steps taken during the day.
2) My Activity – the time spent on moderate and fast activity.
3) My WearTime – the time spent wearing the hearing aids.
4) My Conversations – the frequency of entering active conversations.
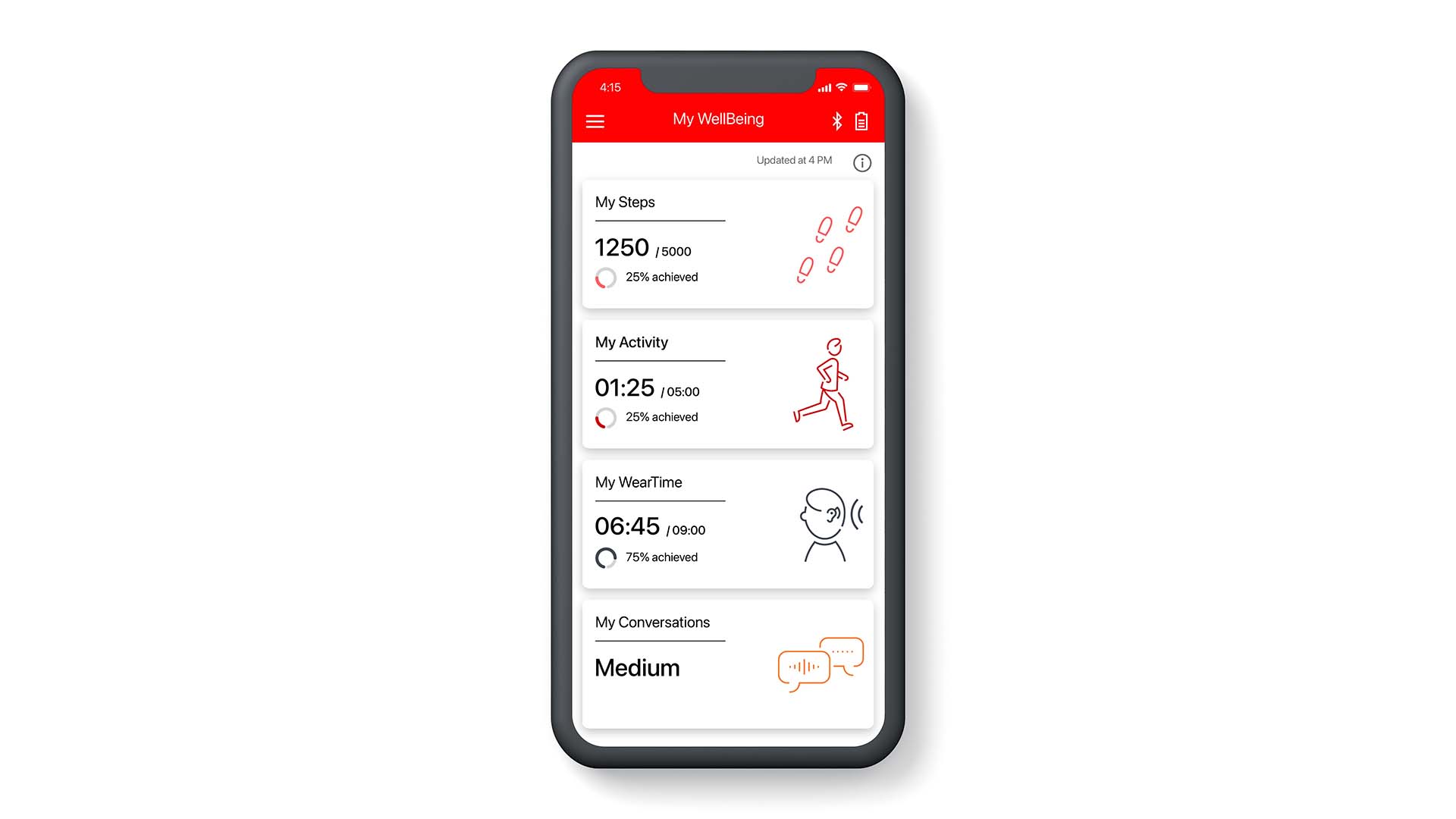
Figure 3. When entering My WellBeing, the wearer immediately gets the current daily status on the four outcome measures. More detailed information on the features is reached by selecting the feature of interest (see Figure 4).
The first two features, My Steps and My Activity, are utilizing the accelerometer (motion sensor) in Signia AX, which tracks all motions of the wearer’s head. Continuous analysis of the motion pattern allows detection of both steps taken and levels of physical activity. The My Activity feature can detect and distinguish between moderate activity (like walking or moving around in the house or garden) and fast activity (like jogging or running). The two features are comparable to similar features available in smartwatches, smartphones and dedicated fitness trackers – but as opposed to these other solutions, My WellBeing doesn’t require wearing another piece of hardware. Wearing the hearing aids is enough. Furthermore, as shown in a later section, the sensor position on the ear allows for a more accurate step count and activity tracking than a tracking device worn on the wrist.
The My WearTime feature indicates the wear time of the hearing aids by registering the time they have been switched on. This allows the wearer to take ownership and monitor the wear time of their hearing aids daily, between visits to the HCP, and thereby strengthening the overall hearing aid benefit. By providing an objective and accurate measurement, My WearTime addresses the fact that hearing aid wearers often tend to overestimate their own wear time (e.g., Laplante-Lévesque et al., 2014).
The My Conversations feature provides an indication of the frequency in which the wearer engages in active conversations. It registers how much the wearer has been exposed to situations where speech is present and where the wearer speaks themselves. The own voice detection is made possible by utilizing the Own Voice Processing 2.0 in Signia AX to determine when the wearer is actively engaged in a conversation. The more active conversations the wearer engages in during the day, the higher the measurement will be on the four-point scale, which goes from “Low” to “Very high”. Thus, the outcome is not an exact time (in hours or minutes), but an average measure of activity for the day. While a daily measure is provided, which shows the difference between socially active and socially less-active days, the primary benefit of this feature is the ability to see changes in activity levels over time. It allows the wearer to see how (or if) the use of hearing aids affects their engagement in conversations over time. In previous research, it has been shown that Own Voice Processing encourages wearers to be more active in communication situations, due to the improved sound of their own voice (Powers et al., 2018). With My WellBeing, wearers can track these changes themselves without the direct involvement of the HCP.
For the first three features, the entry screen (Figure 3) includes information about how close the wearer is to achieving their individual daily goal. This allows the wearer to easily check their daily status when My WellBeing is used as a motivational tool, e.g., to improve their daily activity. (Setting a daily goal is voluntary, and wearers who prefer not to set a goal only see a preset value.) For My Conversations, setting a daily goal is not an option for the same reason as mentioned above; it is designed to be a tool to track changes over time, not one that meets a specified daily target.
For each feature, it is possible to enter a dedicated screen with detailed information. Figure 4 shows examples of these screens for each of the four features. For all features, it is possible to see the history of outcomes over time – at the levels of days, weeks, months, and years. For the first three features, this is also where the daily goal can be set or modified.
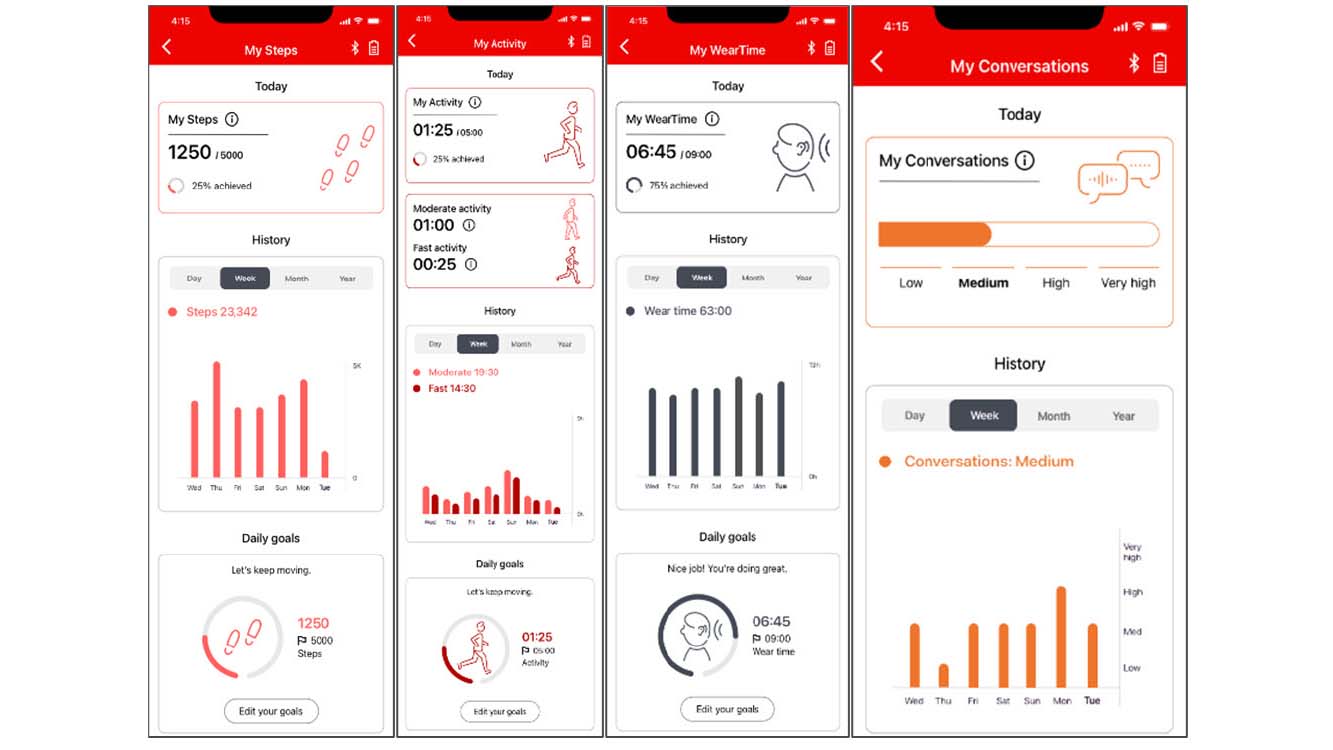
Figure 4. Detailed information provided for each of the four My WellBeing features. The wearer can see the current daily status, the history (data shown for days, weeks, months or years) and compare to (and set) the daily goal for each feature (except from My Conversations).
Obviously, all four features only provide valid data for the time periods where the hearing aids are turned on and worn, so the accuracy and relevance of the displayed measures will depend on how much the hearing aids are worn. This could be an added motivator for individuals who wear their hearing aids in selected situations during the day. To ensure data privacy, all data collected with My WellBeing is only available on the wearer’s smartphone. The HCP will not see the My WellBeing parameters in Connexx.
Positive effects of activity tracking
In Part 1, the many benefits of good hearing and physical activity on general health and well-being were outlined. It became clear that it makes sense to consider (and promote) physical activity when dealing with hearing health. This is indeed the reason for making activity tracking a prominent part of My WellBeing.
Activity tracking has been known for decades and is now easily available in smartwatches, smartphone apps, or in dedicated fitness trackers (often worn on the wrist), and the effects of using activity/fitness trackers have been investigated in many research studies. Systematic reviews and meta-analyses of the studies indicate that devices offering tracking of physical activity – such as the features provided by My WellBeing – have an effect (Tang et al., 2020; Larsen et al., 2022; Ferguson et al., 2022), with the use of self-tracking being associated with higher levels of physical activity.
There is, of course, a lot of individual variability of the effectiveness of activity trackers. For some wearers, the effects may be substantial, while for others, the effects may be small or non-existent. Many factors play a role in the overall effectiveness of activity tracking but a central one is the motivation of the individual wearer. If not motivated to use an activity tracker, the likelihood of non-use becomes high – and if it is not used, it will of course provide no added benefit. This also applies for My WellBeing. Some wearers will easily accept the concept of self-tracking (if they are not into it already). They will have no problems in seeing the potential benefits, and they may be very motivated by setting up personal goals to reach. These wearers will probably be easy to motivate to use My WellBeing.
The situation is likely to be different for the wearers who are less motivated and more reluctant. Some wearers may not be candidates for My WellBeing due to a basic general resistance towards self-tracking. For other wearers, their adoption of My WellBeing may depend on the HCP’s ability to motivate them. By presenting the benefits of maintaining or improving their general health and well-being, which are offered by the hearing aids and further supported by My WellBeing, wearers may become empowered to wear their devices more consistently or be more willing to actively participate in social situations.
Findings from commercial pilot test
The My WellBeing solution has been evaluated in a commercial pilot test in which typical hearing aid wearers were able to use My WellBeing in their everyday life for several months.
The pilot test demonstrated that My WellBeing increased the wearers’ engagement with their hearing aids, as observed by a substantially increased download rate of the app compared to the rate observed without availability of My WellBeing. And once downloaded, the My WellBeing functionality was used. In the survey, approximately 2 out of 3 (64%) of the respondents who had been introduced to My WellBeing and had access to the app reported using it at least once a month during the test period. Only 1 out of 10 indicated that they preferred using their existing fitness tracker.
These findings indicate sizable interest in My WellBeing. However, the pilot test also indicated the HCP plays an important role in how My Wellbeing is perceived and adopted by the wearer. Furthermore, the test unsurprisingly showed that the solution is not for everybody. Some wearers simply do not want to be ‘tracked’ in any way, even if the tracked data never leave their smartphone. Others just prefer to use their hearing aids without using an app, enjoying the audiological benefits provided by the Signia AX platform (Taylor & Jensen, 2022). These benefits are obviously available to the wearer regardless of their opinion of My WellBeing.
Benefits of measuring physical activity at ear level
The position at ear level of the motion sensor used by the My Steps feature to track the steps of the wearer offers some clear benefits compared to activity trackers worn on the wrist. A placement on the wrist can potentially lead to several falsely detected steps when the wearer is moving their arms without taking any steps. A sensor position at the ear is much better suited for not making such (false) detections, while offering very good prerequisites for detecting the real steps taken by the wearer.
In a study with 10 participants, the step counts provided by My Steps were compared to step counts made by two different wrist-worn devices, an Apple Watch Series 7 and a Fitbit Versa3 smartwatch, when all three devices were worn at same time. Each participant wore a set of Signia Pure C&G AX hearing aids while the two other devices were worn on the same arm during testing. The participants were asked to complete four different tasks: A) Taking 200 steps during normal walking, B) Taking 200 steps on a staircase (up and down), C) Filling and emptying a dishwasher for 5 minutes without moving the feet, and D) Moving plates from a table to the upper shelves in a kitchen cabinet (and back) for 5 minutes without moving the feet. In each task, the step reading was registered for each device just before and after the task, and the number of steps taken was calculated as the difference. For more details on the study and the test procedure, see Branda et al. (2022).
The mean number of steps registered with each step counter in each of the four tasks is plotted in Figure 5. For comparison, each plot also indicates the true step count in the task (i.e., 200 steps in tasks A and B, and zero steps in tasks C and D).
Panel A in Figure 5 shows that all three step counters were quite accurate for normal walking. My Steps provided the mean value closest to the true value, but the differences between devices were small and not statistically significant. All mean values were within 4 steps (2%) of the true step count (200), with low variance across participants.
Panel B shows the results from the stairs task. Compared to normal walking, the observed mean deviations from the true step count are slightly larger, but all mean values are within 20 steps (10%) of the true count, and there are no statistically significant differences between the mean values. However, it is still worth noticing that My Steps provides the most accurate mean step count and a substantially lower variance across participants. The latter observation indicates that the individual deviations away from the true value were smaller for My Steps.
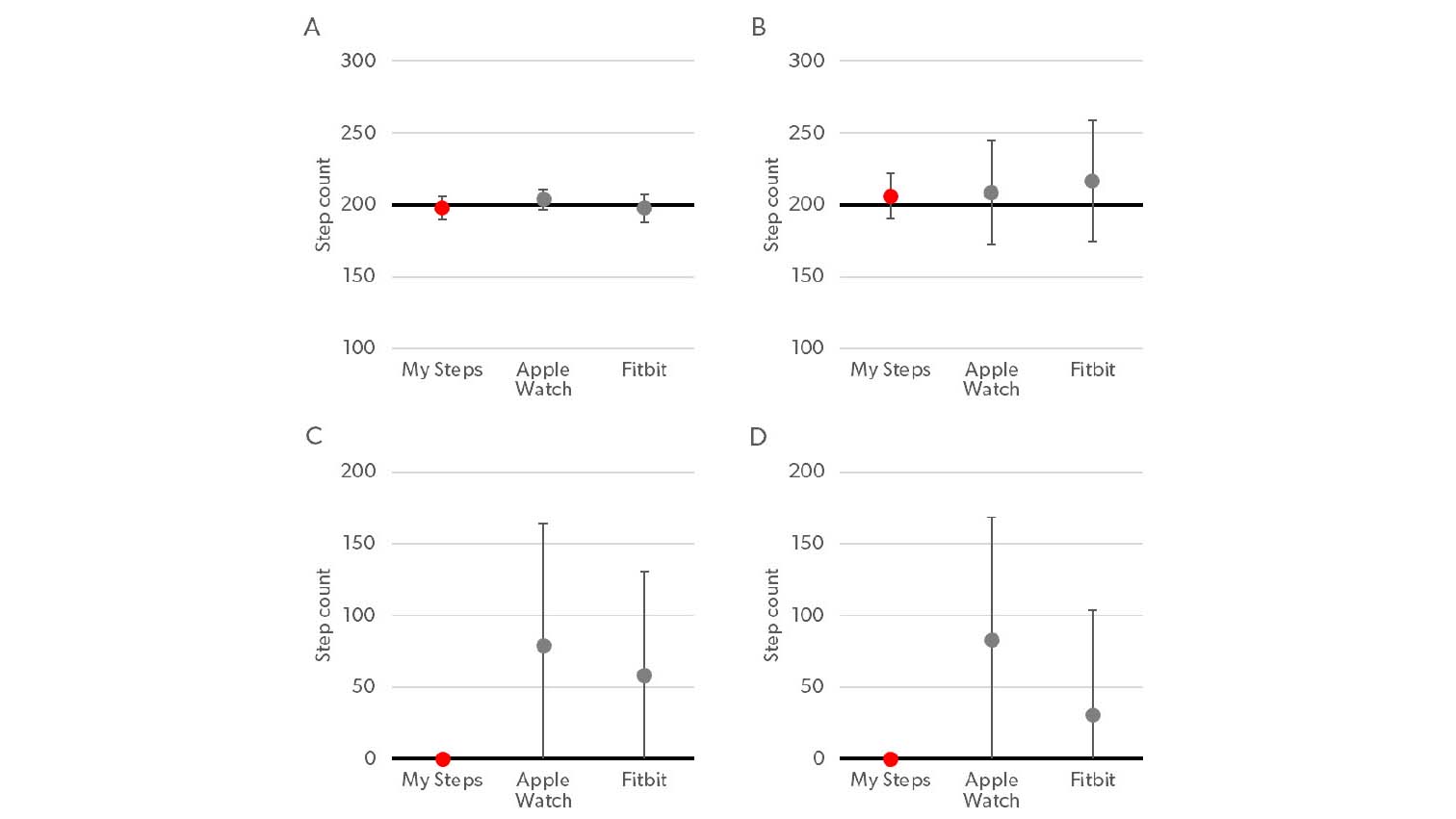
Figure 5. Mean step count for the 10 participants, registered by My Steps and two wrist-worn step counters (Apple Watch and Fitbit) in four tasks: A) Normal walking, B) Walking the stairs, C) Filling/emptying dishwasher, and D) Placing plates on shelves. Error bars indicate ±1 standard deviation. The true step count in each task is indicated by a bold line.
The results from the two tasks where participants did not walk but only moved their arms are shown in panels C and D in Figure 5. The two plots show basically the same pattern. In both tasks, a clear difference between My Steps and the two other devices was observed. Benefitting from the sensor position at the ear, My Steps did not make any (false) detections of steps for any of the participants, resulting in a mean step count (and standard deviation) of 0 steps. In comparison, Apple Watch registered an average of 79 and 83 steps in the two tasks, while the Fitbit device registered an average of 58 and 31 steps. These mean values were significantly higher than the correct count of 0 provided by My Steps. As shown by the error bars in the plots, a large variation across participants was registered for both wrist-worn devices, due in part to the fact that the number of arm movements made during the 5-minute test varied across participants. In just three cases (all observed for Fitbit in task D), a correct step count of 0 was observed with a wrist-worn device.
The false detection of steps made by the wrist-worn step counters suggests that wearing the devices in real life could lead to a lower (but more accurate) step count by My Steps compared to the other devices. To investigate this, the same 10 participants were asked to use the three step counters in their everyday life for one day, from morning till evening. As in the controlled tasks, the participants wore all three devices at the same time, but no true step count was made in this part. The mean number of steps registered by the three devices is plotted together with the standard deviation in the bar graph in Figure 6.
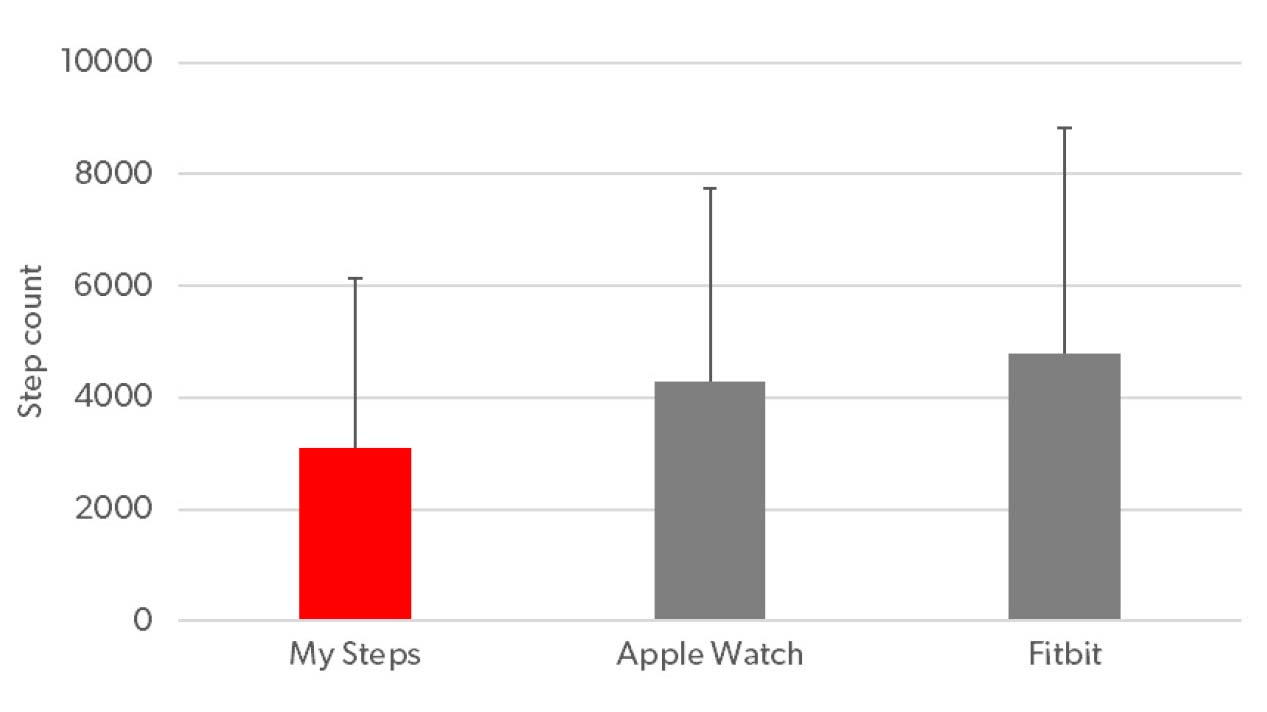
Figure 6. Mean step counts by My Steps and the two wrist-worn devices (Apple Watch and Fitbit) when worn simultaneously for one day. Error bars indicate one standard deviation.
As expected, Figure 6 shows that the mean step count made by the two wrist-worn devices are substantially higher than the count made by My Steps, and in both cases the difference is statistically significant. The Apple Watch count (4,276) is 38% higher than the My Steps count (3,096), while the Fitbit count (4,800) is 55% higher. The large variance indicates, not surprisingly, that the steps taken varied quite a lot across participants. The observed differences in the mean counts suggest that the false step detections observed for the wrist-worn devices accumulate to a substantially large number and add a significant error to the total daily step count when these devices are used in the real world.
In summary, the study showed that while both My Steps and the wrist-worn devices provided accurate step counts for walking in typical situations, My Steps offered a much better protection against false detection of steps in everyday situations in which the wearer moves their arms without taking any steps. This may lead to substantial differences in the step count in everyday life, with My Steps offering more accurate values.
Besides wrist-worn devices, step counters are also readily available as smartphone apps. When the smartphone is carried in an appropriate place, for example in a trouser pocket, it may address the problem of false step detections observed in wrist-worn devices. However, to obtain accurate step counts, it requires the wearer carries the smartphone in all situations during the day, not leaving it on a table or in a bag. From a practical standpoint, for many hearing-aid wearers this would be more cumbersome than having the step counter built into the hearing aids. My Steps offers this distinct advantage.
Summary
This paper summarizes some of the connections between hearing and other health conditions – with a special focus on the effects of hearing loss and use of hearing aids on a person’s general health and well-being. Some of the key messages from the research literature are:
- Hearing loss is associated with many comorbidities and other health-related conditions. The connections are often complex, and all the causal relationships are not fully understood.
- Use of hearing aids does not only improve the ability to hear – but also positively impacts other health conditions, leading to an improved quality of life.
- The more hearing aids are used, the more impact they will have on health and well-being.
- Physical activity has a positive impact on a wide variety of health conditions – many of which are also linked to hearing.
Signia has launched My WellBeing as a tool to support the wearer in maximizing the hearing and general health benefits offered by Signia AX. The tracking features offered by My WellBeing supports the wearer in optimizing the wear time of their hearing aids and in maintaining or even improving the level of their physical and social activity.
My WellBeing is a potential driver of the wearer’s engagement with their hearing aids. Two out of three wearers in the survey stated that they used it on a regular basis.
Physical activity trackers have been shown to be effective in increasing the wearers’ activity levels. The physical activity tracking in My WellBeing benefits from the sensor position at the ear, and the My Steps feature offers a more accurate step count than what is offered by wrist-worn step counters.
References
Abrams H. 2017. Hearing loss and associated comorbidities: What do we know? Hearing Review, 24(12), 32-35.
Alessio H.M. & Marron K.H. 2014. Fitness and Better Hearing, Part 1. Hearing Review, 21(3), 18-24.
Amieva H., Ouvrard C., Giulioli C., Meillon C., Rullier L., et al. 2015. Self-Reported Hearing Loss, Hearing Aids, and Cognitive Decline in Elderly Adults: A 25-Year Study. Journal of the American Geriatrics Society, 63(10), 2099-2104.
Amieva H., Ouvrard C., Meillon C., Rullier L. & Dartigues J.F. 2018. Death, Depression, Disability, and Dementia Associated With Self-reported Hearing Problems: A 25-Year Study. Journals of Gerontology. Series A: Biological Sciences and Medical Sciences, 73(10), 1383-1389.
Arem H., Moore S.C., Patel A., Hartge P., Berrington de Gonzalez A., et al. 2015. Leisure time physical activity and mortality: a detailed pooled analysis of the dose-response relationship. JAMA Internal Medicine, 175(6), 959-967.
Besser J., Stropahl M., Urry E. & Launer S. 2018. Comorbidities of hearing loss and the implications of multimorbidity for audiological care. Hearing Research, 369, 3-14.
Branda E., Jensen N.S. & Warmuth J. 2022. Measuring steps at the ear: How My Steps improves accuracy. Signia White Paper. Retrieved from www.signia-library.com.
Branda E. & Wurzbacher T. 2021. Motion Sensors in Automatic Steering of Hearing Aids. Seminars in Hearing, 42(03), 237-247.
Byun H., Chung J.H., Lee S.H., Kim E.M. & Kim I. 2022. Dementia in a Hearing-impaired Population According to Hearing Aid Use: A Nationwide Population-based Study in Korea. Ear and Hearing, Early Online, 1-8.
Davis H., Schlundt D., Bonnet K., Camarata S., Bess F.H., et al. 2021. Understanding listening-related fatigue: Perspectives of adults with hearing loss. International Journal of Audiology, 60(6), 458-468.
Ferguson M.A., Kitterick P.T., Chong L.Y., Edmondson-Jones M., Barker F., et al. 2017. Hearing aids for mild to moderate hearing loss in adults. Cochrane Database of Systematic Reviews, 9.
Ferguson T., Olds T., Curtis R., Blake H., Crozier A.J., et al. 2022. Effectiveness of wearable activity trackers to increase physical activity and improve health: a systematic review of systematic reviews and meta-analyses. The Lancet Digital Health, 4(8), e615-e626.
Holman J.A., Drummond A. & Naylor G. 2021a. Hearing Aids Reduce Daily-Life Fatigue and Increase Social Activity: A Longitudinal Study. Trends in Hearing, 25.
Holman J.A., Hornsby B.W.Y., Bess F.H. & Naylor G. 2021b. Can listening-related fatigue influence well-being? Examining associations between hearing loss, fatigue, activity levels and well-being. International Journal of Audiology, 60(sup2), 47-59.
Houmøller S.S., Wolff A., Möller S., Narne V.K., Narayanan S.K., et al. 2022. Prediction of successful hearing aid treatment in first-time and experienced hearing aid users: Using the International Outcome Inventory for Hearing Aids. International Journal of Audiology, 61(2), 119-129.
Kuo P.L., Di J., Ferrucci L. & Lin F.R. 2021. Analysis of Hearing Loss and Physical Activity Among US Adults Aged 60-69 Years. JAMA Network Open, 4(4), e215484.
Laplante-Lévesque A., Nielsen C., Jensen L.D. & Naylor G. 2014. Patterns of hearing aid usage predict hearing aid use amount (data logged and self-reported) and overreport. Journal of the American Academy of Audiology, 25(02), 187-198.
Larsen R.T., Wagner V., Korfitsen C.B., Keller C., Juhl C.B., et al. 2022. Effectiveness of physical activity monitors in adults: systematic review and meta-analysis. BMJ, 376, e068047.
Laureyns M., Bisgaard N., Bobeldijk M. & Zimmer S. 2020. Getting the numbers right on Hearing Loss Hearing Care and Hearing Aid Use in Europe A Europe Wide Strategy Joint AEA, EFHOH, EHIMA report. Brussels: EIMA.
Lin F.R. & Ferrucci L. 2012. Hearing loss and falls among older adults in the United States. Archives of Internal Medicine, 172(4), 369-371.
Lin F.R., Metter E.J., O’Brien R.J., Resnick S.M., Zonderman A.B., et al. 2011. Hearing Loss and Incident Dementia. Archives of Neurology, 68(2), 214-220.
Livingston G., Huntley J., Sommerlad A., Ames D., Ballard C., et al. 2020. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. The Lancet, 396(10248), 413-446.
Maharani A., Dawes P., Nazroo J., Tampubolon G. & Pendleton N. 2018. Longitudinal Relationship Between Hearing Aid Use and Cognitive Function in Older Americans. Journal of the American Geriatrics Society, 66(6), 1130-1136.
Martinez-Amezcua P., Powell D., Kuo P.L., Reed N.S., Sullivan K.J., et al. 2021. Association of Age-Related Hearing Impairment With Physical Functioning Among Community-Dwelling Older Adults in the US. JAMA Network Open, 4(6), e2113742.
Pedersen B.K. & Saltin B. 2015. Exercise as medicine – evidence for prescribing exercise as therapy in 26 different chronic diseases. Scandinavian Journal of Medicine and Science in Sports, 25 Suppl 3, 1-72.
Powell D.S., Oh E.S., Reed N.S., Lin F.R. & Deal J.A. 2022. Hearing Loss and Cognition: What We Know and Where We Need to Go. Frontiers in Aging Neuroscience, 13.
Powers T.A., Davis B., Apel D. & Amlani A.M. 2018. Own Voice Processing Has People Talking More. Hearing Review, 25(7), 42-45.
Rumalla K., Karim A.M. & Hullar T.E. 2015. The effect of hearing aids on postural stability. Laryngoscope, 125(3), 720-723.
Samocha-Bonet D., Wu B. & Ryugo D.K. 2021. Diabetes mellitus and hearing loss: A review. Ageing Research Reviews, 71, 101423.
Sanders M.E., Kant E., Smit A.L. & Stegeman I. 2021. The effect of hearing aids on cognitive function: A systematic review. PloS One, 16(12), e0261207.
Schacht J., Talaska A.E. & Rybak L.P. 2012. Cisplatin and aminoglycoside antibiotics: hearing loss and its prevention. The Anatomical Record: Advances in Integrative Anatomy and Evolutionary Biology, 295(11), 1837-1850.
Shield B. 2019. Hearing Loss – Numbers and Costs. Evaluation of the social and economic costs of hearing impairment. Report for Hear-It AISBL. Brunel University London.
Smith R. 2008. The end of disease and the beginning of health. BMJ Group Blogs.
Tan H., Lan N., Knuiman M., Divitini M., Swanepoel D., et al. 2018. Associations between cardiovascular disease and its risk factors with hearing loss—a cross‐sectional analysis. Clinical Otolaryngology, 43(1), 172-181.
Tang M.S.S., Moore K., McGavigan A., Clark R.A. & Ganesan A.N. 2020. Effectiveness of Wearable Trackers on Physical Activity in Healthy Adults: Systematic Review and Meta-Analysis of Randomized Controlled Trials. JMIR Mhealth Uhealth, 8(7), e15576.
Taylor B. & Jensen N.S. 2022. Evidence Supports the Advantages of Signia AX’ s Split Processing. Signia White Paper. Retrieved from www.signia-library.com.
Thomson R.S., Auduong P., Miller A.T. & Gurgel R.K. 2017. Hearing loss as a risk factor for dementia: a systematic review. Laryngoscope investigative otolaryngology, 2(2), 69-79.
Tye-Murray N., Spry J.L. & Mauzé E. 2009. Professionals with hearing loss: Maintaining that competitive edge. Ear and Hearing, 30(4), 475-484.
Warburton D.E., Nicol C.W. & Bredin S.S. 2006. Health benefits of physical activity: the evidence. Canadian Medical Association Journal, 174(6), 801-809.
Weinstein B.E., Sirow L.W. & Moser S. 2016. Relating Hearing Aid Use to Social and Emotional Loneliness in Older Adults. American Journal of Audiology, 25(1), 54-61.
WHO 1948. Constitution of the World Health Organization. Geneva: World Health Organization.
WHO 1997. WHOQOL: Measuring Quality of Life. Geneva: World Health Organization.
WHO 2017. Global costs of unaddressed hearing loss and cost-effectiveness of interventions. Geneva: World Health Organization.
WHO 2020. WHO guidelines on physical activity and sedentary behaviour. Geneva: World Health Organization.
WHO 2021. World report on hearing. Geneva: World Health Organization.
Williger B. & Lang F.R. 2015. Hearing aid use in everyday life: managing contextual variability. Gerontology, 61(2), 158-165.
Wong L.L., Hickson L. & McPherson B. 2003. Hearing aid satisfaction: what does research from the past 20 years say? Trends in Amplification, 7(4), 117-161.


